
Built for the road
Skai brings healthcare that moves with transportation and telecom workers, reaching them wherever the job takes them.
Learn more about Built for the road
Solutions at Skai are pointing national employers in an exciting new direction: flexible and tailored to the needs of each client and workforce.

Skai brings healthcare that moves with transportation and telecom workers, reaching them wherever the job takes them.
Learn more about Built for the road
For the workers behind every counter and checkout line, Skai makes healthcare that fits real life.
Learn more about Built for the floor
Skai is transforming healthcare for the manufacturing workforce by delivering proactive, flexible support that keeps teams healthy, productive and on the line.
Learn more about Built for the line
Skai has built healthcare for frontline workers that’s flexible, accessible and designed to meet them where they are.
Learn more about Built for the shift
Your health plan like never before. Illume brings data, clarity and smart insights together to help you make confident, strategic decisions.
Learn more about Skai Spotlight: Illume
Meet Celeste: a first-of-its-kind health navigation company that connects members to everything they need to take care of their health.
Learn more about Skai Collaboration Spotlight: Celeste
Skai Blue Cross Blue Shield has decades of expertise supporting the complex health needs of high-turnover populations. Let’s take a look at how our approach supports frontline workers’ health.
Learn more about Improving health outcomes for America’s frontline workers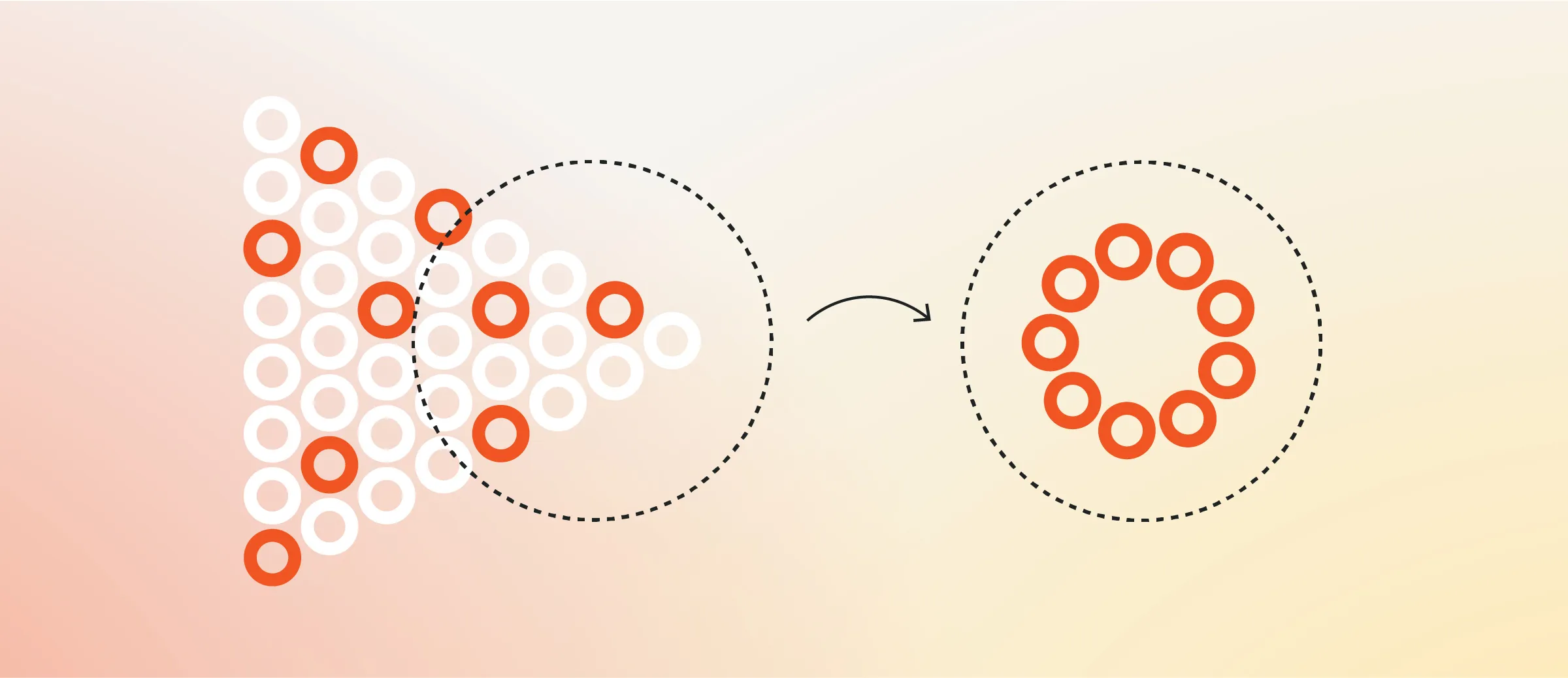
Skai Blue Cross Blue Shield’s health solution Celeste makes integration a reality and allows employers and members to get the most out of their point solutions.
Learn more about Celeste makes point solution integration a reality
We’re raising the bar in healthcare with a new plan purpose-built for national employers who expect more than the status quo.
Learn more about Things are looking up: Introducing SkaiThere's so much more to Skai. See how we'll change the way you think about healthcare.
Let's connect